News
Marler Clark has published 5,598 articles about foodborne illness outbreaks and lawsuits.
Current Outbreaks
April 17, 2024
Trader Joe's Basil link in Salmonella Outbreak
CDC, public health and regulatory officials in several states, and the U.S. Food and Drug Administration (FDA) are collecting different types of data to investigate a multistate outbreak of Salmonella...
March 23, 2024
February 16, 2024
All Articles
November 24, 2023 • Case News
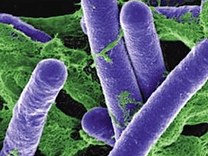
When To Consider Antibiotics for Listeria
Listeriosis is usually a self-limited illness—which means that most infected individuals will improve without the need for medical care. But for those patients with a high fever, a stool culture and antibiotic-treatment may be justified for otherwise healthy individuals. Although there have been no studies done to determine what drugs …

November 24, 2023 • Case News
Common Myths and Misconceptions About E. coli
E. coli is often referred to as the best or most-studied free-living organism. More than 700 serotypes of E. coli have been identified. The “O” and “H” antigens on the bacteria and their flagella distinguish the different serotypes. It is important to remember that most kinds of E. coli bacteria …

November 24, 2023 • Case News
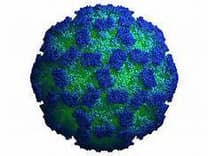
A Brief Look at Supportive Therapy for Hepatitis A
Once a clinical infection is established, there is no specific treatment for hepatitis A. Affected individuals generally suffer from loss of appetite, so the main concern is ensuring a patient receives adequate nutrition and avoids permanent liver damage. An individual’s perception of the severity of fatigue or malaise is the …

November 04, 2023 • Case News
TMP/SMX: What They Are and Why They're Important
Trimethoprim-sulfamethoxazole (TMP-SMX), also known as co-trimoxazole, is a combination of two antimicrobial agents that act synergistically against a wide variety of bacteria. It is commonly used to treat urinary tract infections, middle ear infections, bronchitis, traveler’s diarrhea, and shigellosis (bacillary dysentery). TMP-SMX is also used to prevent or treat Pneumocystis …
November 04, 2023 • Case News
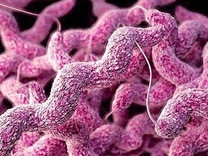
How Macrolides Help You Fight Campylobacter Infections
According to the CDC, macrolides like azithromycin are the current drugs of choice when antibiotic treatment is indicated for Campylobacter infections. The resistance to macrolides in Campylobacter has remained stable. …
November 04, 2023 • Case News
What To Do If You Think You've Contracted Botulism
Although botulism can be diagnosed based on clinical symptoms, distinguishing it from other diseases is often difficult, especially in the absence of other known persons affected by the condition. Common misdiagnoses include Guillain-Barré syndrome and myasthenia gravis, which also manifest flaccid paralysis. …
November 04, 2023 • Case News
How Long Do the Effects of Norovirus Last?
Norovirus illness usually develops 24 to 48 hours after ingestion of contaminated food or water. Symptoms typically last a relatively short amount of time, approximately 24 to 48 hours. These symptoms include nausea, vomiting, diarrhea, and abdominal pain. Headache and low-grade fever may also accompany this illness. People infected with …
November 02, 2023 • Events & Speaking Engagements
China International Food Safety & Quality Conference (2023)
Bill Marler, a food safety attorney, attended the opening of this conference, serving as a panelist. The theme of the discussion centered on the challenges of foodborne diseases. Yuki Minato from the World Health Organization, moderated the discussion. The other panelists included: …
September 30, 2023 • Firm News
When To Consider Legal Action for Food Poisoning
I have been litigating foodborne illness cases for three decades. The key to my success has been to find a quick, reliablemethod of distinguishing between legitimate food poisoning claims and suspect ones. The key is causation – did the food product cause the illness. If you can prove causation, you …

September 30, 2023 • Firm News
Tips To Help Prevent Salmonella Poisoning
In general, safe cooking and preparation of food can kill existing Salmonella bacteria and prevent it from spreading. Additionally, safe choices at the grocery store can greatly reduce the risk of Salmonella. …

September 30, 2023 • Firm News
Salmonella vs. Listeria: What's the Difference?
Salmonella is a bacterium that causes one of the most common enteric (intestinal) infections in the United States – salmonellosis. Listeria is a gram-positive rod-shaped bacterium that can grow under either anaerobic (without oxygen) or aerobic (with oxygen) conditions. …
September 30, 2023 • Firm News
What are the Advancements in the Diagnosis of Cyclospora
Cyclosporiasis is usually diagnosed symptomatically in clinical settings, including the presence of watery diarrhea, abdominal cramping, and bloating. In untreated, immunocompetent people, the diarrhea can last from days to weeks to a month or more and can wax and wane, with variable oocyst shedding. Oocysts can continue to be shed …
August 23, 2023 • Outbreaks
Listeria outbreak: Three die after drinking contaminated milkshakes
Three people have died, and three others are in hospital after drinking milkshakes contaminated with listeria bacteria in the US state of Washington, health officials say. Marler Clark, the Listeria attorneys, have been retained by a family of a man who died in the Frugals Listeria outbreak. …

August 18, 2023 • Publications
What Not to Eat: A Food Safety Expert's Guide to Eating Safely
With this in mind, the BBC spoke to food safety expert Bill Marler, a lawyer who has been involved in practically every major food poisoning case in the United States over the last few decades. Here’s what he does and doesn’t eat. …

August 18, 2023 • Publications
Food safety advocates support USDA proposal to protect consumers from Salmonella in some processed chicken proucts
For years CSPI and advocates like food safety lawyer Bill Marler have urged USDA to do a better job of controlling Salmonella in poultry, including by asking the agency to prioritize banning certain more dangerous strains or amounts of Salmonella. …

August 17, 2023 • Press Releases
Marler Clark Files First Lawsuit in Salmonella Outbreak Linked to Papa Murphy’s Cookie Dough
Seattle, WA – Today Marler Clark filed a Salmonella lawsuit against Papa Murphy’s, representing Michael Williams and Renee Sanders who were victims of an outbreak linked to Chocolate Chip Cookie and S’mores Bar dough. (See complaint below) The CDC reported that this outbreak sickened 26 people in six states: California …

August 15, 2023 • Case News
Tips For Preventing Your Dog from Giving You Campylobacter
Summertime for many means more time spent outside with our family, friends, and often our four-legged companions. It is a wonderful time of year to exercise ourselves, and mankind’s best friend, but as dog owners we need to remember that caring for our pets often necessitates caring for ourselves. While …

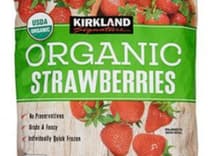
August 14, 2023 • Press Releases
Marler Clark Files Hepatitis A Lawsuits: Costco’s Kirkland Brand Frozen Strawberries Sicken Customers
Seattle, WA – The hepatitis A attorneys at Marler Clark, a Seattle based law firm, filed lawsuits against Scenic Fruit Company, LLC (berry grower) and Californica Splendor, Inc. (berry distributor), on behalf of Tanna Mosalsky and Ryan Darrow. Costco sold Kirkland Signature frozen organic strawberries linked to a multi-state hepatitis …
August 01, 2023 • Case News
Norovirus and kids – the perfect mix
It happens at least once a year—the dreaded norovirus wave at daycare. The first year I was cavalier, thinking, “We’ll be the lucky ones who dodge it.” We most certainly weren’t. And neither was any other family in our cohort, as far as I know. …

July 21, 2023 • Press Releases
Marler Clark Retained by Family of Deceased Listeria Victim
Tacoma-Pierce County Health Department announced a Listeria outbreak in Western Washington which resulted in three deaths from an unknown source. Marler Clark, a law firm specializing in foodborne illness litigation, is representing the family of a victim in this tragic outbreak. …
July 17, 2023 • Case News
What are the Long-Term Health Effects of Salmonella Infection?
Another dangerous complication is bacteremia, which affects approximately 5% of infected individuals. If the Salmonella bacteria enters a person’s bloodstream (bacteremia), it can infect tissues throughout the body. The bacteria can cause a focal infection, where it becomes localized in a tissue and causes an abscess, arthritis, endocarditis, or other …

July 12, 2023 • Outbreaks
2011 Listeria Outbreak Linked to Cantaloupes: A History
A total of 148 persons infected with any of the five (5) outbreak-associated strains of Listeria monocytogenes were reported to CDC from 28 states. The number of infected persons identified in each state was as follows: Alabama (1), Arkansas (1), California (4), Colorado (40), Idaho (2), Illinois (4), Indiana (3) …

July 12, 2023 • Case News
How To Detect Botulism in Canned Foods at Home
Follow proper canning instructions. Inspect the canning container for any leaks, bulges, cracks, or damages. If they are present, do not consume the product. If the container spurts liquid or foam when opened do not consume the product. Discard the food if it has a spoiled smell, color, or texture …

July 12, 2023 • Case News
Why E. coli Outbreaks happen not just in Beef
Although foods of bovine origin are the most common cause of both outbreaks and sporadic cases of E. coli O157:H7 infections, outbreaks of illnesses have been linked to a wide variety of food items. For example, produce has been the source of substantial numbers of outbreak-related E. coli O157:H7 infections …

July 12, 2023 • Case News
The Health Effects of Cyclospora Exposure
Cyclospora infects the small intestine (bowel) and usually causes watery diarrhea, bloating, increased gas, stomach cramps, and loss of appetite, nausea, low-grade fever, and fatigue. In some cases, vomiting, explosive diarrhea, muscle aches, and substantial weight loss can occur. Some people who are infected with Cyclospora do not have any …

Food Safety Resources
Salmonella Food Poisoning
What is Salmonella and how does it cause food poisoning? The term Salmonella refers to a specific group of gram-negative bacteria with the potential to …
The Incidence of Salmonella Infections
Typhoidal Salmonella Salmonella enterica serotypes Typhi, Sendai, and Paratyphi A, B, or C are found exclusively in humans. These serotypes, collectively referred to as typhoidal …
The Prevalence of Salmonella in Food and Elsewhere
Most Salmonella infections are caused by eating contaminated food. One study found that 87% of all confirmed cases of Salmonella are foodborne. Foods of animal …
